Cardiovascular Imaging (CMR & CCT) and Interventional Cardiology,
Institut universitaire de cardiologie et de pneumologie de Québec;
Faculty of Medicine, Université Laval, Québec, QC, Canada
eric.larose@criucpq.ulaval.ca

The Typical Catheterization Laboratory Patient is Changing
Traditionally, patients admitted to the catheterization laboratory have displayed typical risk factors for atherosclerosis, including advancing age, smoking, diabetes, dyslipidemia, hypertension or a family history of premature coronary artery disease. The contemporary interventionalist is confronted by a growing population of patients with only 1 or even no traditional risk factors, corresponding to a moderate or low probability of coronary artery disease based on traditional risk scores. Over two-thirds of younger adults presenting with acute myocardial infarction would not be considered high risk for coronary events if assessed using the National Cholesterol Education Program-Adult Treatment Panel III criteria [1]. In the recent EASY trial of over 1,000 all-comer patients undergoing coronary angioplasty, waist circumference was greatly increased to a mean 99 ± 5 cm despite a mean body mass index of 28 ± 5 kg/m2, indicating overweight but not obesity. This "abdominally obese" population of a mean age of 60 years had relatively low incidences of traditional risk factors, including 30% smoking, 50% hypertension and 15% diabetes.
Key Points
- Traditional risk factors do not explain the full spectrum of risk in patients assessed in the catheterization laboratory.
- Atherosclerosis risk is related to underlying biology and not merely to luminal stenosis severity.
- Ectopic adipose tissue may partly explain the atherosclerosis risk observed in catheterization laboratory patients who do not have traditional risk factors.
Back To Basics: At-Risk Atherosclerosis
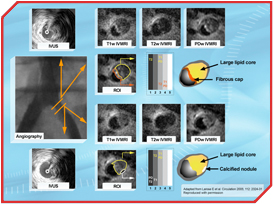
Atherosclerosis biology, more than stenosis severity, determines risk for coronary events, including unstable angina, myocardial infarction and sudden coronary death. While angioplasty in myocardial infarction reduces events, the interventionalist must face the harsh reality that angioplasty in stable coronary artery disease reduces angina symptoms but does not prevent acute coronary syndrome. The plaque at risk for thrombotic events has typical features, including a lipid-rich necrotic core, thin fibrous cap, active inflammation and at times an overhanging thrombus. Imaging methods based on magnetic resonance imaging, ultrasound backscatter, optical coherence tomography, computed tomography and thermography have shown promise in better identifying at-risk biology and potentially broadening therapies based on atherosclerosis risk beyond atherosclerosis morphology (Figure) [2].
 [Click to enlarge]
[Click to enlarge]
Ectopic Adipose Tissue and Atherosclerosis
Increased intra-abdominal (visceral) adipose tissue is related to an increase in atherosclerosis risk factors. Coronary events also rise as intra-abdominal adipose tissue increases. A similar relationship to risk factors and atherosclerosis has been suggested with visceral adipose tissue on the surface of the heart. A lifestyle modification program that included increased physical activity/exercise and healthy eating habits (SYNERGIE trial) was found to generate significant reductions in ectopic intra-abdominal adipose tissue. The interventional cardiologist must remember that beyond traditional risk factor management, novel metabolic risk factors respond to lifestyle modifications. Patient motivation and adherence to a healthy lifestyle may be greatly improved by appropriate counselling from the interventional cardiologist when the patient is "all ears" following coronary angioplasty.
The typical patient treated in the interventional cardiology laboratory is changing. Focus is shifting towards therapy of atherosclerosis beyond mere stenosis, and the contribution of metabolic risk factors in addition to traditional risk factors is recognized. The role of the interventional cardiologist in targeting the appropriate patients for lifestyle modification cannot be overstated.
References
- Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486-97.
- Larose E, Yeghiazarians Y, Libby P, et al. Characterization of human atherosclerotic plaques by intravascular magnetic resonance imaging. Circulation 2005; 112: 2324-31.



